INTRODUCTION
Circulatory System, or cardiovascular system, in
humans, the combined function of the heart, blood, and
blood vessels to transport oxygen and nutrients to organs and tissues throughout
the body and carry away waste products. Among its vital functions, the
circulatory system increases the flow of blood to meet increased energy demands
during exercise and regulates body temperature. In addition, when foreign
substances or organisms invade the body, the circulatory system swiftly conveys
disease-fighting elements of the immune system, such as white blood
cells and antibodies, to regions under attack. Also, in the case of
injury or bleeding, the circulatory system sends clotting cells and proteins to
the affected site, which quickly stop bleeding and promote healing.
| Phagocytes |
Most animals have systems that resist
disease. The disease resistance provided by these systems is called immunity.
There are two types of immunity: innate and adaptive. Innate, or
nonspecific, immunity is the body’s first, generalized line of defense
against all invaders. Innate immunity is furnished by barriers such as
skin, tears, mucus, and saliva, as well as by the
rapid inflammation of tissues that takes place shortly
after injury or infection. These innate immune mechanisms hinder
the entrance and spread of disease but can rarely prevent disease
completely.
If an invader gets past this first line of
defense, the cells, molecules, and organs of the immune system develop
specifically tailored defenses against the invader. The immune system can call
upon these defenses whenever this particular invader attacks again in the
future. These specifically adapted defenses are known as adaptive, or
specific, immunity.
Adaptive immunity has four distinguishing
properties: First, it responds only after the invader is present. Second, it is
specific, tailoring each response to act only on a specific type of invader.
Third, it displays memory, responding better after the first exposure to an
invader, even if the second exposure is years later. Fourth, it does not usually
attack normal body components, only those substances it recognizes as
nonself.
Adaptive immune responses are actually
reactions of the immune system to structures on the surface of the invading
organism called antigens. There are two types of adaptive immune
responses: humoral and cell mediated. During humoral immune responses,
proteins called antibodies, which can stick to and
destroy antigens, appear in the blood and other body fluids.
Humoral immune responses resist invaders that act outside of cells,
such as bacteria and toxins (poisonous substances produced by
living organisms). Humoral immune responses can also prevent viruses from
entering cells.
`During cell-mediated immune
responses, cells that can destroy other cells become active. Their
destructive activity is limited to cells that are either infected with, or
producing, a specific antigen. Cell-mediated immune responses resist invaders
that reproduce within the body cells, such as viruses. Cell-mediated responses
may also destroy cells making mutated (changed) forms of normal
molecules, as in some cancers.
COMPONENTS OF THE IMMUNE SYSTEM
The ability of the immune system to mount a response to disease is dependent on
many complex interactions between the components of the immune system and the
antigens on the invading pathogens, or disease-causing agents.
White blood cells are the mainstay of the immune system. Some white blood cells,
known as macrophages, play a function in innate immunity by surrounding,
ingesting, and destroying invading bacteria and other foreign organisms in a
process called phagocytosis (literally, “cell eating”), which is part of
the inflammatory reaction. Macrophages also play an important role in adaptive
immunity in that they attach to invading antigens and deliver them to be
destroyed by other components of the adaptive immune system.
 |
| Lymphocytes creating antibodies |
Lymphocytes are specialized white
blood cells whose function is to identify and destroy invading antigens. All
lymphocytes begin as “stem cells” in the bone marrow, the soft tissue
that fills most bone cavities, but they mature in two different places. Some
lymphocytes mature in the bone marrow and are called B lymphocytes. B
lymphocytes, or B cells, make antibodies, which circulate
through the blood and other body fluids, binding to antigens and helping to
destroy them in humoral immune responses.
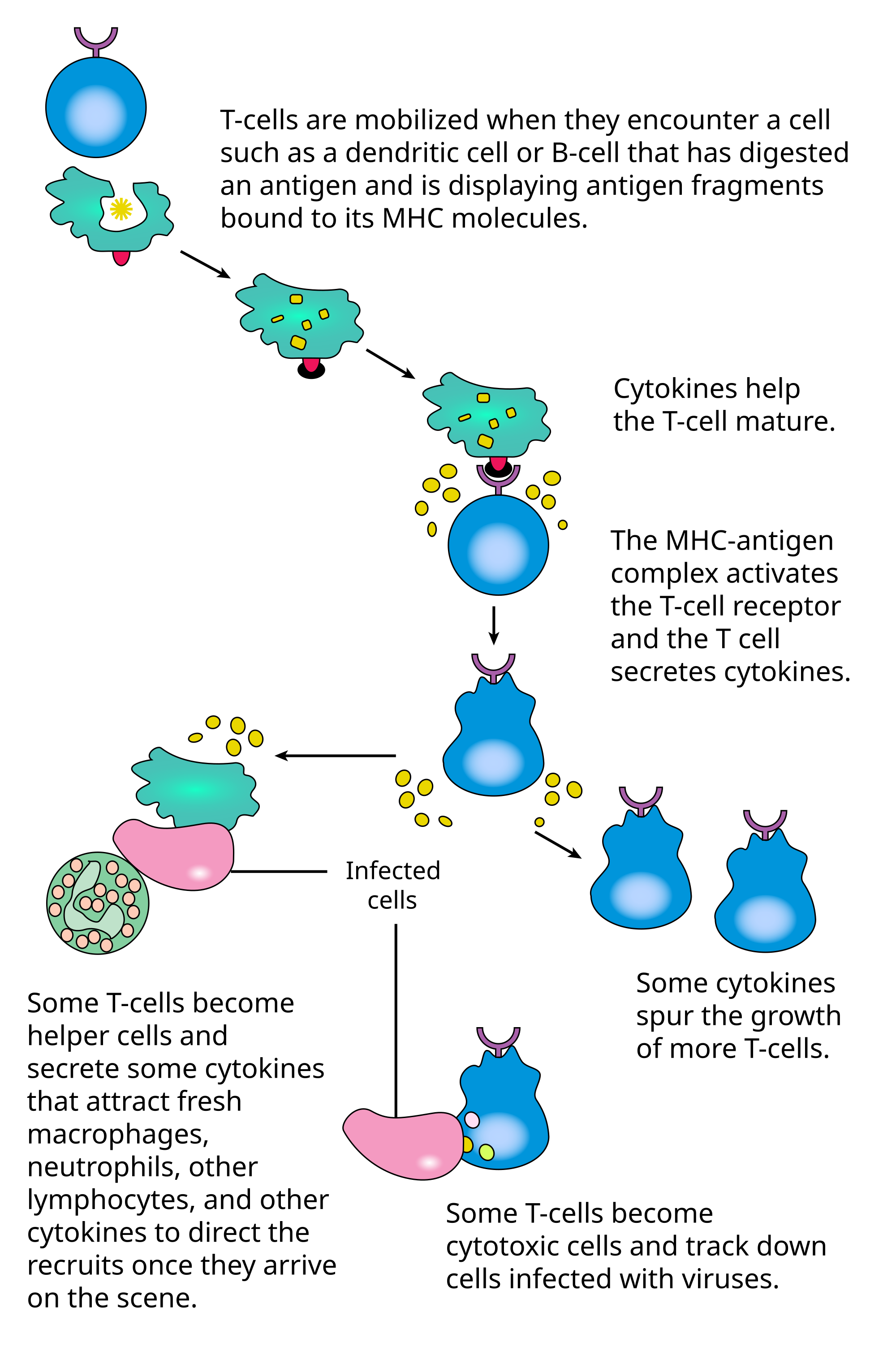
Other lymphocytes, called T
lymphocytes, or T cells, mature in the thymus, a small
glandular organ located behind the breastbone. Some T lymphocytes, called
cytotoxic (cell-poisoning) or killer T lymphocytes, generate
cell-mediated immune responses, directly destroying cells that have specific
antigens on their surface that are recognized by the killer T cells. Helper T
lymphocytes, a second kind of T lymphocyte, regulate the immune system by
controlling the strength and quality of all immune responses.
Most contact between antigens and
lymphocytes occurs in the lymphoid organs—the lymph nodes, spleen, and
tonsils, as well as specialized areas of the intestine and lungs. Mature lymphocytes constantly travel through
the blood to the lymphoid organs and then back to the blood again. This
recirculation ensures that the body is continuously monitored for invading
substances.
Antigen Receptors
One of the characteristics of adaptive immunity is that it is specific: Each response is tailored to a specific type of invading antigen. Each lymphocyte, as it matures, makes an antigen receptor—that is, a specific structure on its surface that can bind with a matching structure on the antigen like a lock and key. Although lymphocytes can make billions of different kinds of antigen receptors, each individual lymphocyte makes only one kind. When an antigen enters the body, it activates only the lymphocytes whose receptors match up with it.
Antigen-Presenting Cells
When an antigen enters a body cell, certain transport molecules within the cell attach themselves to the antigen and transport it to the surface of the cell, where they “present” the antigen to T lymphocytes. These transport molecules are made by a group of genes called the major histocompatibility complex (MHC) and are therefore known as MHC molecules. Some MHC molecules, called class I MHC molecules, present antigens to killer T cells; other MHC molecules, called class II MHC molecules, present antigens to helper T cells.
HUMORAL IMMUNE RESPONSE
The humoral immune response involves a complex series of events after antigens
enter the body. First, macrophages take up some of the antigen and attach it to
class II MHC molecules, which then present the antigen to T helper cells. The T
helper cells bind the presented antigen, which stimulates the T helper cells to
divide and secrete stimulatory molecules called interleukins. The
interleukins in turn activate any B lymphocytes that have also bound the
antigen. The activated B cells then divide and secrete antibodies. Finally, the
secreted antibodies bind the antigen and help destroy it.
ANTIBODIES
Antibodies are Y-shaped proteins
called immunoglobulins (Ig) and are made only by B cells. The antibody binds to
the antigen at the ends of the arms of the Y. The area at the base of the Y
determines how the antibody will destroy the antigen. This area is used to
categorize antibodies into five main classes: IgM, IgG, IgA, IgD, and IgE.
During the humoral immune response, IgM is the first class of antibody made.
After several days, other classes appear. Exactly which other Ig classes a B
cell makes depends on the kind of interleukins it receives from the T helper
cells.
Antibodies can sometimes stop an antigen’s
disease-causing activities simply by neutralization—that is, by binding
the antigen and preventing it from interfering with the cell’s normal
activities. For example, the toxin made by tetanus bacteria binds
to nerve cells and interferes with their control of muscles. Antibodies against
tetanus toxin stick to the toxin and cover the part of it that binds to nerve
cells, thereby preventing serious disease. All classes of antibodies can
neutralize antigens.
Antibodies also help destroy antigens by
preparing them for ingestion by macrophages in a process called opsonization. In
opsonization, antibodies coat the surface of antigens. Since macrophages
have receptors that stick to the base of the antibody’s Y structure, antigens
coated with antibodies are more likely to stick to the macrophages and be
ingested. Opsonization is especially important in helping the body resist
bacterial diseases.
Finally, IgM and IgG antibodies can
trigger the complement system, a group of proteins that cause cells to
disintegrate by cutting holes in the cell membrane. Complement is important in
resisting bacteria that are hard to destroy in other ways. For example, some of
the bacteria that cause pneumonia have a slimy coating, making it
hard for macrophages to ingest and eliminate them. However, if IgM and IgG
antibodies bind to the pneumonia bacteria and activate the complement system, it
is able to cut holes in the bacteria to destroy them.
Although the IgM and IgG classes of
antibodies work best in the circulatory system, IgA can exit the bloodstream and
appear in other body fluids. IgA is thus important in preventing infection at
mucosal surfaces, such as the intestine and the lung.
Since these are the sites where most infectious agents enter, IgA is
particularly important in resistance to many diseases. IgA is also found in
mother’s milk and may help nursing newborns resist disease.
CELL-MEDIATED IMMUNE RESPONSE
As with the humoral immune response, the cell-mediated immune response involves
a complex series of events after antigens enter the body. Helper T cells are
required, so some of the antigen must be taken up by macrophages and presented
to helper T cells. The helper T cells bind the presented antigen and thereby
become activated to divide and secrete interleukins. The interleukins in turn
activate any killer T cells that have already bound antigen attached to class I
MHC molecules on infected cells. The activated killer T cells can then kill any
cells displaying antigen attached to class I MHC molecules, effectively
eliminating any cells infected with the antigen.
When the body is first exposed to an antigen, several days pass before the adaptive immune response becomes active. Immune activity then rises, levels off, and falls. During following exposures to the same antigen, the immune system responds much more quickly and reaches higher levels. Because the first, or primary, immune response is slow, it cannot prevent disease, although it may help in recovery. In contrast, subsequent, or secondary, immune responses usually can prevent disease because the pathogen is detected, attacked, and destroyed before symptoms appear. This complete resistance to disease is called immunity and may be achieved through either active or passive immunization.
A. Active Immunization
Active immunization occurs when a
person’s own immune system is activated and generates a primary immune response.
Active immunization can be triggered in two ways, either by natural immunization
or by vaccination.
In natural immunization, the body
contracts a disease and recovers. Because a primary immune response occurs
during the illness, the immune system will mount a disease-preventing secondary
response every time it is subsequently exposed to the disease. Natural
immunization is developed during childhood diseases, such as chicken
pox. After having had the disease once, a person is no longer susceptible
to it.
Vaccination is intentional
immunization against a particular disease by the use of vaccines,
substances that are structurally similar to the actual disease-producing agents
but that do not produce disease themselves. Most vaccines take one of two forms.
The first type of vaccine, such as the vaccines for tetanus and whooping
cough, contains chemically killed bacteria or other pathogenic organisms.
The other type, such as the oral polio vaccine, contains weakened
forms of living organisms that have been genetically selected so they do not
produce disease.
B. Passive
Immunization
Another way to provide immunity is by
means of passive immunization. Passive immunization does not engage the
person’s own immune system. Instead, the individual receives antibodies that
were created in another person or animal. Such antibodies can be lifesaving when
a disease progresses too rapidly for natural immunization to occur. For example,
if a person who has not been immunized against tetanus bacteria is exposed to
tetanus, the toxin produced by these bacteria would reach a deadly level before
a primary immune response could begin. Administering antibodies against tetanus
toxin quickly neutralizes the toxin and prevents death.
Passive immunization has two drawbacks:
First, the person does not mount an active immune response, so the immunizing
effect is temporary and the person is not immune after recovery. Second, if
passive immunization is used repeatedly, it occasionally produces side
effects
IMMUNE SYSTEM DISORDERS
The immune system recognizes and attacks
anything different from the substances normally present within an individual,
even substances that are only slightly different, such as transplanted tissues
and organs.
When an organ is transplanted, the MHC of
the donor organ is recognized as foreign and attacked by the recipient’s immune
system. To minimize the chances of transplant rejection, physicians seek
transplant donors who share as many MHC genes as possible with the transplant
recipient. Even then, most transplant recipients are given drugs to suppress
their immune response and prevent rejection of the transplant.
If the transplanted tissue contains T
lymphocytes from the donor, as in bone marrow transplants, these donor T
lymphocytes may recognize the recipient’s tissues as foreign and attack them.
Physicians can reduce or prevent this potentially fatal graft-versus-host
(GVH) reaction by removing all mature T lymphocytes from the organ or tissue
before performing the transplant.
DEFICIENCY
Deficiencies in immune function may be
either inherited or acquired. Inherited immune deficiencies usually reflect the
failure of a gene important to the generation or function of immune system
components.
Some inherited diseases damage a person’s
innate immunity by making macrophages incapable of ingesting or breaking down
invading organisms. Individuals affected by these diseases are especially
susceptible to opportunistic infections—that is, infections by normally
harmless organisms that can flourish in a person whose immune system has been
weakened.
DiGeorge syndrome is an inherited immune
disorder in which a person has no thymus and, therefore, cannot produce mature T
lymphocytes. People with this disorder can mount only limited humoral immune
responses, and their cell-mediated immune responses are severely limited.
The most extreme example of a hereditary
immune deficiency is severe combined immunodeficiency (SCID). Individuals with
this disease completely lack both T and B lymphocytes and thus have no adaptive
immune responses. People with SCID must live in a completely sterile
environment, or else they will quickly die from infections.
Acquired immune deficiencies can be
caused by infections and also other agents. For example, radiation therapy and some kinds of drugs used in treating
disease reduce lymphocyte production, resulting in damaged immune function.
People undergoing such therapies must be carefully monitored for lowered immune
function and susceptibility to infections. Environmental and lifestyle factors,
such as poor nutrition or stress, can also affect the immune system’s general
status.
An infectious agent resulting in fatal
immune deficiency is the human immunodeficiency virus (HIV). This
virus causes acquired immunodeficiency syndrome (AIDS) by infecting
and eventually destroying helper T cells. Because helper T cells regulate all
immune responses, their loss results in an inability to make adaptive immune
responses. This complete lack of immune function makes individuals with AIDS
highly susceptible to all infectious agents.















